If you are concerned about a suspicious lesion or mole, seeking immediate advice from a qualified healthcare practitioner is vital. This section of the app helps guide you through: taking appropriate action, the referral criteria used in UK general practice, the process used by skin specialists to diagnose skin cancer and an overview of treatment and staging.
If you are concerned about a lesion or mole then you should get them checked as soon as possible by a doctor. You should first make an appointment to see your GP who will perform a skin check, examine any lesions or moles of concern and if needed, refer you to a skin specialist / dermatologist for professional clinical assessment. Alternatively you may wish to have concerns checked privately by a consultant dermatologist.
MAKING AN APPOINTMENT WITH YOUR GP
It’s a good idea when making your appointment to ask if there is a doctor at your practice that has a specialist interest in skin cancer. Some GPs have more knowledge about skin cancer than other GPs who may have had very little training in this subject.
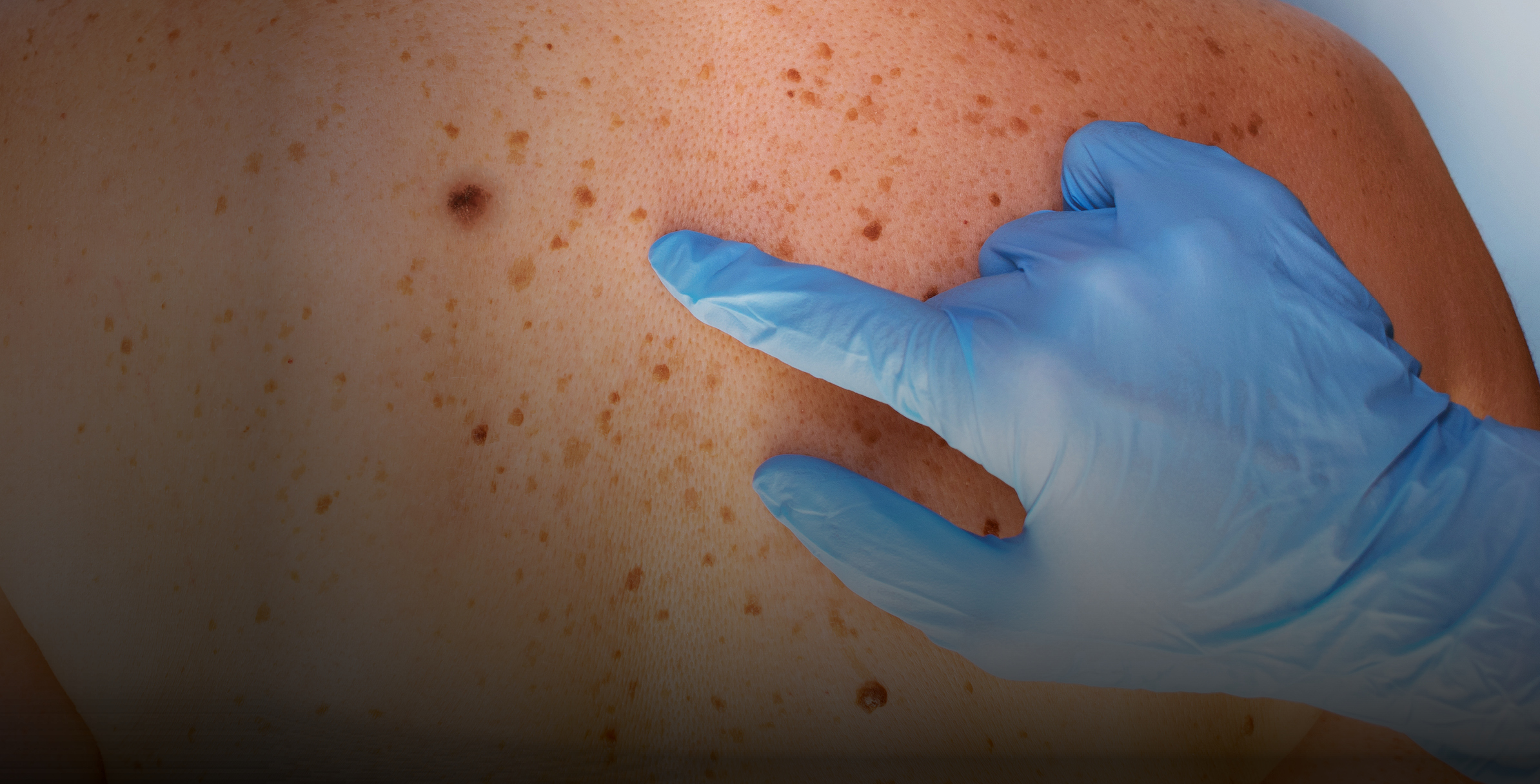
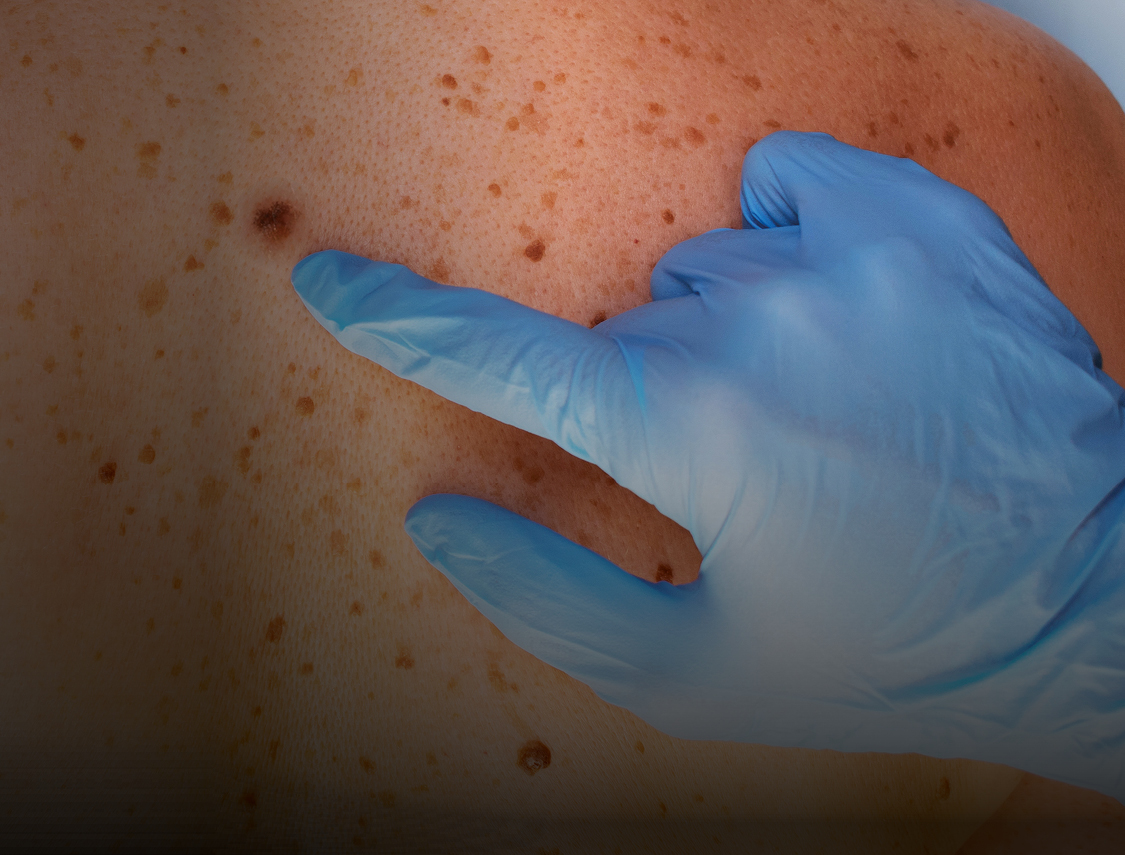
Some GPs with a specialist interest in skin cancer will be trained to use a dermatoscope - a hand-held instrument, a bit like a magnifying glass that is used to examine the area very closely. This does not hurt or affect your skin.
DURING AN APPOINTMENT WITH YOUR GP
Your doctor should be familiar with your history and during your appointment they will talk to you about risk factors and your family history to help them determine your level of risk for the development of skin cancer. If you have used this app to generate your own risk assessment, you can show it to your doctor to help communicate your level of risk.
If you have taken photographs of your suspicious lesion or mole you should show them to your doctor to help communicate your concerns along with any notes you have made with regards to dates, sizes and changes in appearance or sensation.
It is important that you feel satisfied with the outcome of your GP appointment. Unfortunately most GPs have very little training in dermatology, so it is not uncommon for skin cancers, including melanoma (the most serious form) to be misdiagnosed.
To help you assess your level of satisfaction based on the outcome of your appointment, it’s useful to understand the referral process that GPs use to determine whether or not you should be referred to a dermatologist for appropriate clinical assessment. This process is outlined below using the weighted 7-point check list.
If you decide that you are not happy with the outcome of your appointment, you should either; make another appointment to discuss your concerns further; ask to see a different doctor for a second opinion; or consider booking a private consultation with a dermatologist.


When making referral decisions, your doctor may use the weighted 7-point checklist which has been recommended by NICE (National Institute for Health and Care Excellence) for routine use in UK general practice, as follows:
All suspicious pigmented skin lesions that score 3 points or more using this check list should be referred urgently (within 2 weeks) to a dermatologist for professional clinical assessment.
MAJOR FEATURES OF THE LESION (2 points each):
MINOR FEATURES OF THE LESION (1 point each):
Patients should also be referred urgently (within 2 weeks) if dermoscopy suggests melanoma skin cancer and if a pigmented or non-pigmented skin lesion is suggestive of nodular melanoma or other forms of rarer skin cancers.
Your GP should also refer you if you are taking medicines or have a medical condition that lowers your immune system.
Squamous Cell Carcinoma (SCC)
If a SCC is suspected, an urgent cancer pathway referral (for an appointment within 2 weeks) should be made by you GP.
Basal Cell Carcinoma (BCC)
If a BCC is suspected a routine referral (non-urgent referral) should be made, unless your doctor is particularly concerned that a delay in treatment may have a significant impact due to factors such as lesion size or location - for example larger lesions on the face or close to the eye.
Despite this guidance, please be aware that in the UK there is a huge shortage of dermatologists who are under a great deal of pressure to cope with increasing numbers of NHS referrals. If you are experiencing delays, or want to see a specialist sooner, you may wish to consider booking a private consultation.
Due to demand, booking a private consultation with dermatology services local to you, may or may not decrease your waiting time, so you would need to research this before making a decision. However there are other options available that can significantly speed up this process and even remove the need to first visit your GP - such as the My Skin Doctor App.


In 2020 Skcin partnered with My Skin Doctor and the UK’s largest dermatology practice to launch the self-pay version of their patient-led App which allows UK patients (regardless of their postcode) to access dermatology services immediately – without first having to wait to be referred to a dermatologist by their GP.
The My Skin Doctor App allows users to take and upload photographs of any skin condition to a growing team of experienced Consultant Dermatologists who provide expert, swift and efficient triage, with patients receiving a personalised care plan including a diagnosis (where possible), information about their condition and an effective treatment plan within 3 working days! Furthermore, this information is simultaneously communicated to the patient’s GP and included in patient records.
With a 100% Clinical Governance record, 100% GP satisfaction and fully GDPR compliant, My Skin Doctor is meeting current and future patient needs, whilst ensuring quality of care is not compromised and access is equitable across the UK.
A self-pay consultation of a suspect lesion, mole or other skin condition costs £75, £5 of which is donated to Skcin to support our vital work undertaken to prevent skin cancer and promote early detection across the UK.
To download the app or find out more visit: https://www.myskindoctor.co.uk/


When you are referred to a skin specialist (a dermatologist or specialist plastic surgeon) by your GP, they should be able to confirm the diagnosis by carrying out a physical examination. If you have used the risk assessment tool within this app, it’s a good idea to share this information with them.
They may also perform a biopsy, a minor surgical procedure where either part or all of the tumour is removed and studied under a microscope. This is usually carried out under local anaesthetic. A biopsy allows the specialist to determine the type of skin cancer you have and whether there is any chance of it spreading to other parts of your body.
Basal Cell Carcinoma (BCC)
If you are diagnosed with basal cell carcinoma (the most common form of all skin cancers) and the tumour has been removed and tested, further tests aren’t usually required as it’s very unlikely that the cancer will spread.
Squamous Cell Carcinoma (SCC)
If you are diagnosed with squamous cell carcinoma (the second most common form of skin cancer), further tests may be needed because in rarer cases it can spread to other parts of the body.
Treatment for non-melanoma skin cancer
Surgery is the main treatment for non-melanoma skin cancer. This involves removing the cancerous tumour and some of the surrounding skin. Other non-surgical treatments for non-melanoma skin cancer as well as pre-cancerous skin lesions include: cryotherapy, anti-cancer creams, photodynamic therapy (PDT), radiotherapy, chemotherapy and/or electrochemotherapy. Overall, treatment is successful for at least 9 out of 10 people with non-melanoma skin cancer.


Diagnosis of melanoma is relatively uncommon and can only be confirmed after a full professional assessment, appropriate biopsy, histological examination and specialist interpretation. If your dermatologist or skin specialist suspects a melanoma they may remove the mole (excision biopsy) and send it for examination by a histopathologist (a specialist who examines tissue) to check whether it is cancerous.
A biopsy is usually carried out under local anaesthetic. If a melanoma is confirmed another operation is usually required, most often performed by a plastic surgeon or dermatologist to remove a wider area of skin.
Staging of melanoma
‘Staging’ is the process of determining the size / depth of the melanoma and if / how far it has spread. It is used to determine how serious the cancer is and how best to treat it.
When the melanoma is removed, the depth of the tumour will be examined. This is the depth (measured in mm) from the surface of the skin at which the cancer cells are present at the time of surgical excision.
The earliest stage melanomas are stage 0 (melanoma in situ), and then range from stages I (1) through IV (4). Some stages are split further, using capital letters (A, B, etc.).
As a rule, the lower the number, the less the cancer has spread and the higher the number, the more the cancer has spread. Within a stage, an earlier letter means a lower stage. Most melanoma are less than 1mm thick and are less likely to grow back or require further treatment.
Further tests and treatments.
Further tests will be carried out if there is a concern the cancer has spread into other organs, bones or bloodstream. Patients with melanoma will be cared for by a team of specialists that should include: a dermatologist, a plastic surgeon, an oncologist, a pathologist and a specialist nurse.
When helping patients decide on their treatment, the team will consider: the type of cancer, the stage of the cancer and the patient’s general health. The team will then recommend what they believe to be the best treatment option.
The NHS have further information on the treatments for the various stages of melanoma.


Remember, the sooner a skin cancer is identified and treated, the better a person’s chance of avoiding surgery, or in the case of a serious melanoma, potential disfigurement or even death.
Equally, when it comes to skin cancer, prevention is better than cure and the good news is that around 90% of cases are preventable by adopting simple sun safe practices.
Please use the various sections within this app that have been developed to empower you to take charge of your personal and your family’s skin health and surveillance as follows: