- Pre-cancerous skin lesions that are slow growing with the potential to develop into cancer.
- Commonly found on areas frequently exposed to the sun such as the head, neck, back of hands & forearms.
- Usually appear as small brown, pink or whitish, scaly, red, single or multiple rough spots, smaller than 1cm in diameter.
- They can feel rough and cause soreness, irritation, discomfort or pain, or may just pose a cosmetic nuisance.
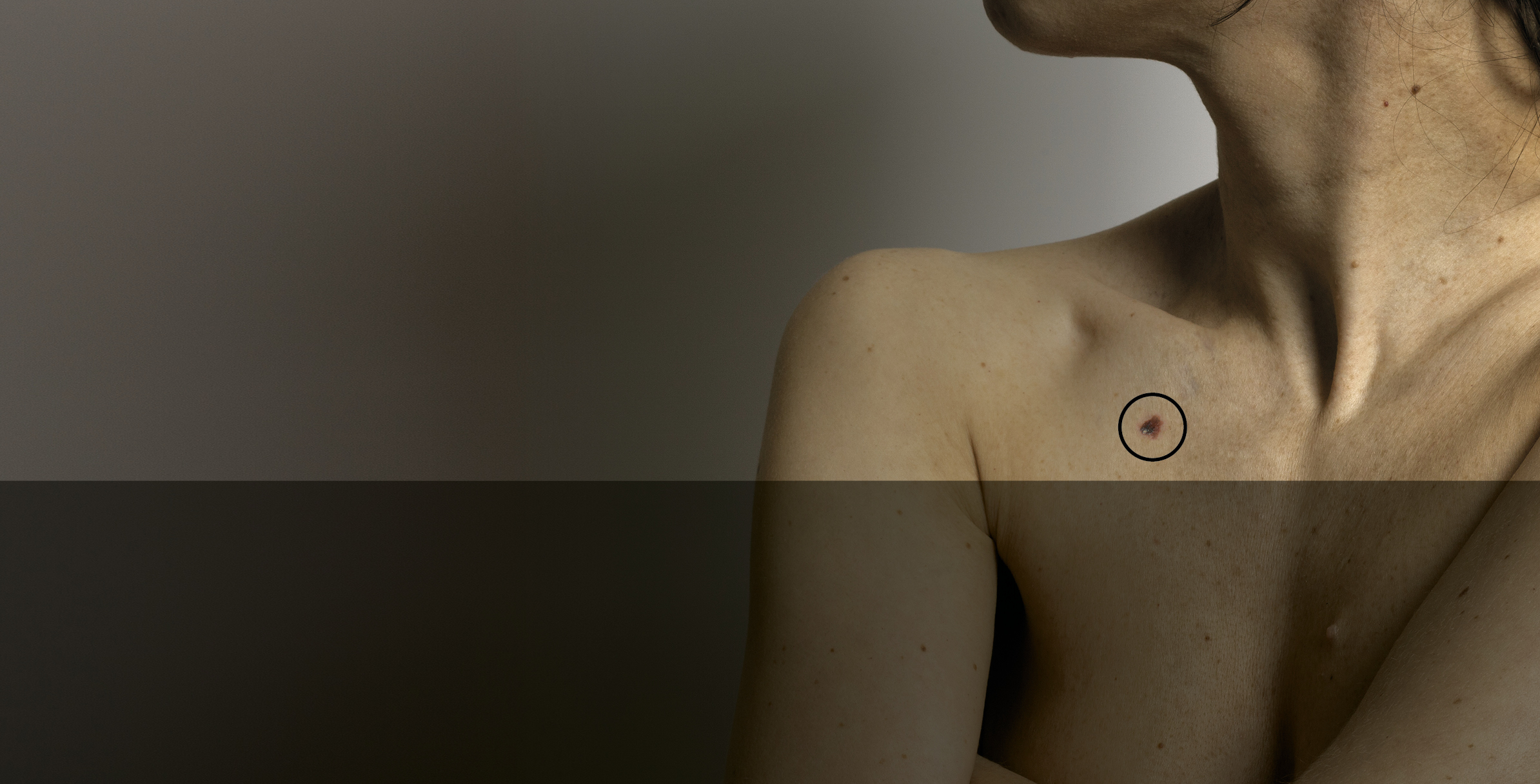
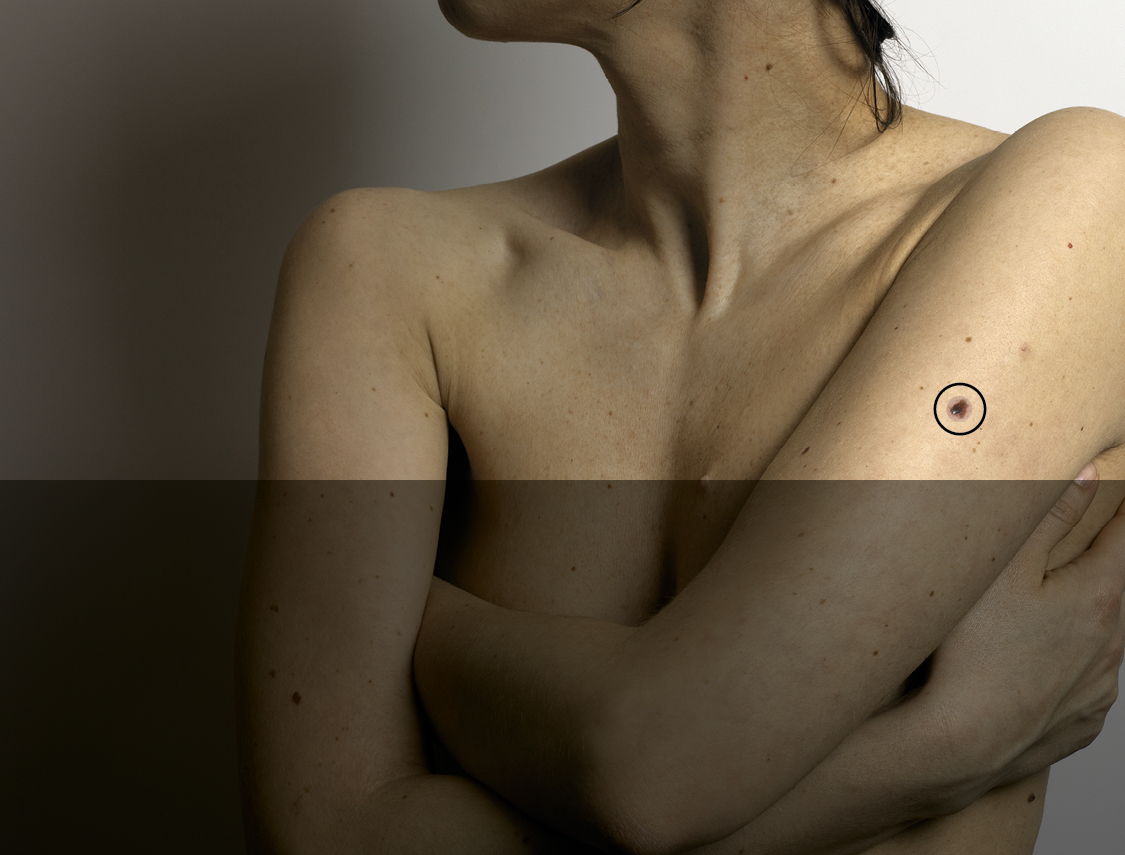
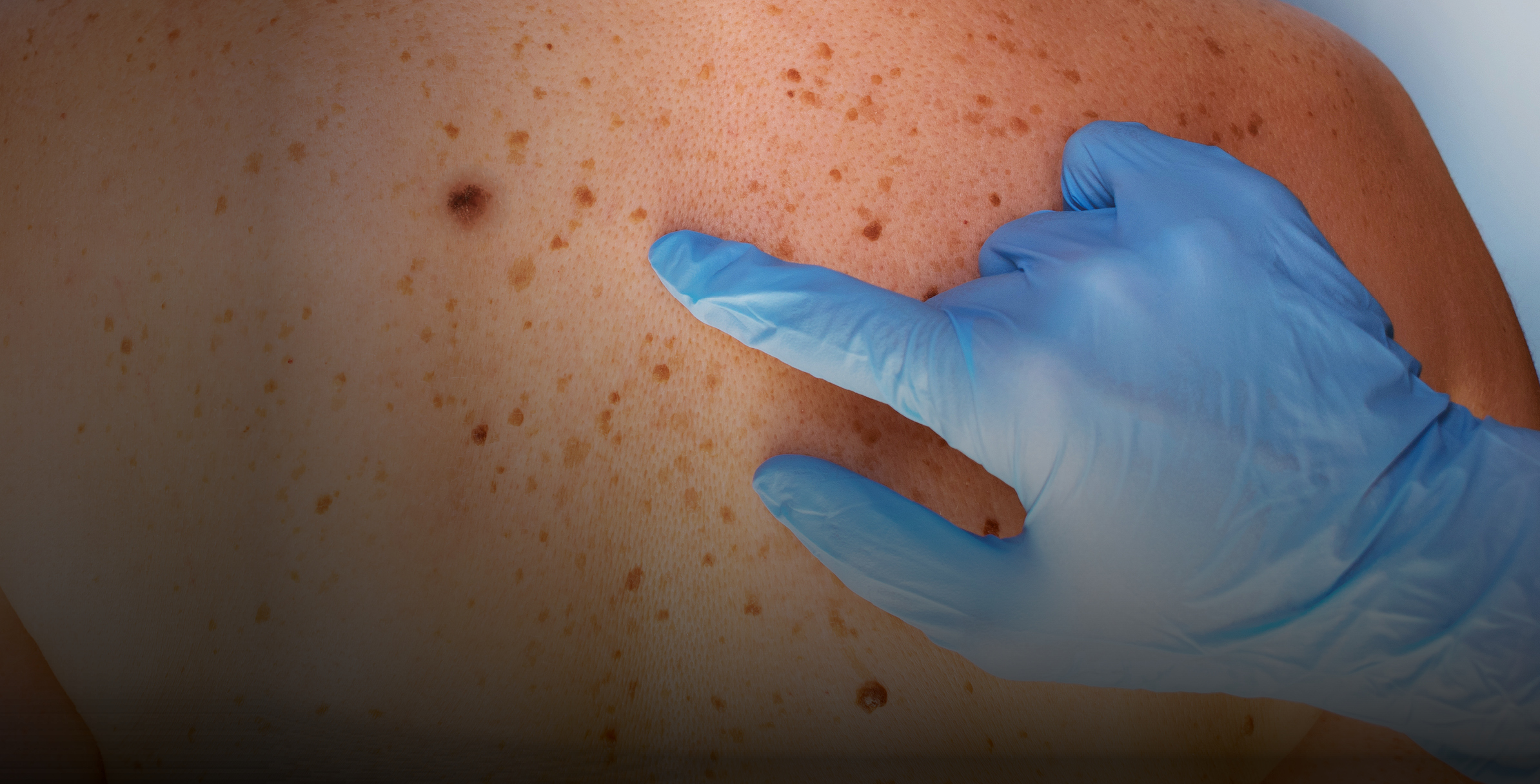
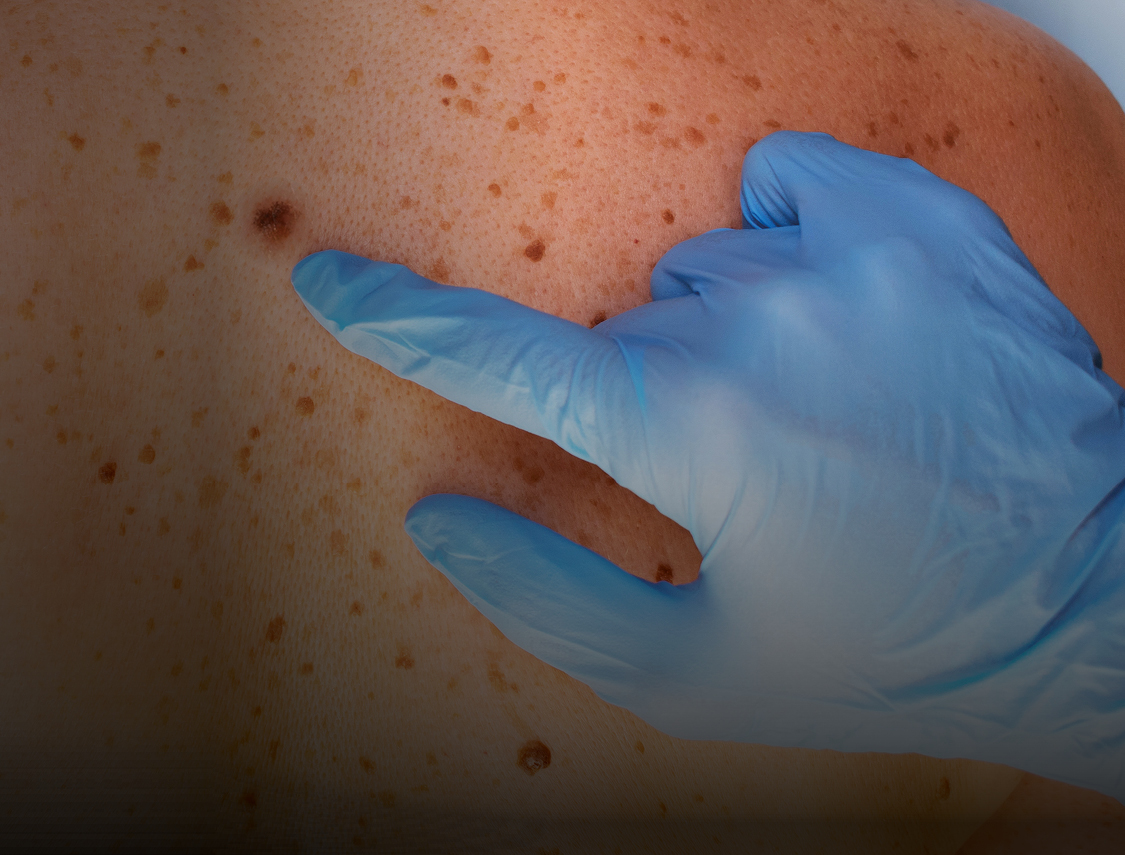
- Importance of Skin Surveillance
- Introduction to Skin Cancer
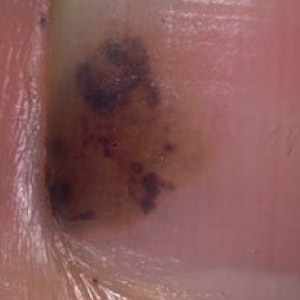
- Skin Cancer in Skin of Colour
- Pre-Cancerous Skin Lesions
- Non-Melanoma Skin Cancer
- Melanoma Skin Cancer
- Take Action Check List
- Taking action with concerns
- The weighted 7-point checklist
- My skin doctor app
- Confirming diagnosis (nmsc)
- Confirming diagnosis (mm)
- Knowledge is power
- Spotted a Skin Cancer?
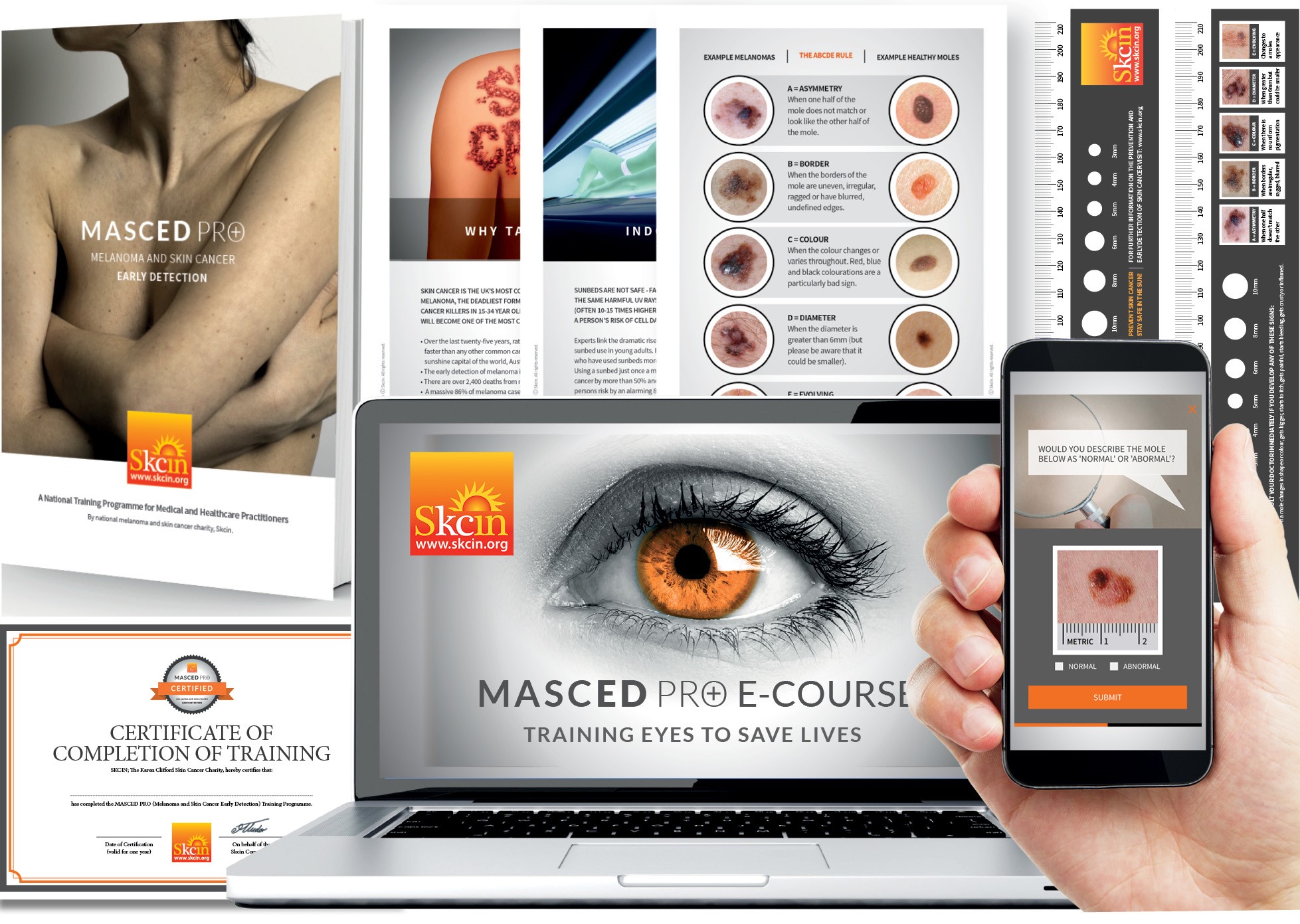
- Masced Training
Install
- Importance of Skin Surveillance
- Introduction to Skin Cancer
- Skin Cancer in Skin of Colour
- Pre-Cancerous Skin Lesions
- Non-Melanoma Skin Cancer
- Melanoma Skin Cancer
- Take Action Check List
- Taking action with concerns
- The weighted 7-point checklist
- My skin doctor app
- Confirming diagnosis (nmsc)
- Confirming diagnosis (mm)
- Knowledge is power
- Spotted a Skin Cancer?
- Masced Training